Understanding Mental Health: A Comprehensive Guide
Understanding Mental Health: What It Is, Why It Matters, and How to Take Care of It
Mental health affects everything—how we think, how we feel, how we connect, and how we cope. It influences our relationships, our decisions, our stress levels, and our ability to enjoy life. Yet despite being such a vital part of our overall well-being, mental health is often overlooked or misunderstood.
This guide breaks down what mental health really means, explores common mental health conditions, and offers practical tools to support your mental wellness—whether for yourself or someone you care about.
What Is Mental Health?
Mental health is our emotional, psychological, and social well-being. It’s how we process feelings, manage stress, relate to others, and make daily choices. Just like physical health, we all have mental health—and taking care of it is just as important.
Mental Health ≠ Mental Illness
A key distinction: having mental health doesn’t mean having a mental illness. Everyone has mental health, but not everyone experiences a mental health disorder. And just like you can have a cold or a chronic condition physically, mental illnesses vary in intensity and duration.
Having good mental health doesn’t mean never feeling sad or anxious. It means being able to cope with life’s ups and downs, build relationships, and recover from difficult experiences with resilience.
FAQ: Is mental illness permanent?
Not always. Many mental health conditions can be treated or managed with the right support—therapy, medication, lifestyle changes, and community. Recovery is possible.
Common Mental Health Conditions
1. Depression
Depression is more than feeling sad or “down.” It’s a medical condition that impacts your energy, motivation, memory, relationships, and even your physical health. It can make simple tasks—like getting out of bed, eating, or replying to a text—feel overwhelming.
There are several types of depression:
Major Depressive Disorder (MDD): Persistent low mood lasting for at least two weeks, often with no obvious cause.
Persistent Depressive Disorder (Dysthymia): A chronic form of depression with symptoms that may be less intense but last for years.
Seasonal Affective Disorder (SAD): Depression that occurs seasonally, often in winter months due to reduced sunlight.
Postpartum Depression: A serious condition affecting birthing parents after childbirth, distinct from “baby blues.”
Depression can distort how you see yourself and the world around you. It may tell you that you’re a burden, that nothing will get better, or that your efforts don’t matter. But these thoughts are symptoms—not truths. With support and treatment, depression is highly manageable, and many people recover fully.
Therapies that help: CBT, interpersonal therapy, EMDR (if trauma-related), medication, and lifestyle changes like exercise and structured routine.
2. Anxiety Disorders
Anxiety is our body’s natural alarm system—but for some, that alarm rings too often or too loudly, even when there’s no real threat.
Anxiety disorders aren’t just about “worrying too much.” They often come with intense physical symptoms—racing heart, dizziness, sweating, or gastrointestinal distress—and can significantly interfere with daily functioning.
Types of Anxiety Disorders:
Generalized Anxiety Disorder (GAD): Chronic worry about everyday situations—often feeling like you can’t “turn your brain off.”
Panic Disorder: Sudden, intense episodes of fear (panic attacks) that may feel like a heart attack or loss of control.
Social Anxiety Disorder: Deep fear of being judged, embarrassed, or humiliated in social situations.
Specific Phobias: Irrational fear of a particular object or situation (e.g., heights, flying, needles).
Separation Anxiety Disorder (in adults too): Extreme distress at the thought of being away from loved ones or safe environments.
Left untreated, anxiety can become self-reinforcing. You may begin to avoid people, places, or activities that trigger symptoms—shrinking your life in the process. Fortunately, anxiety responds well to treatment.
Therapies that help: CBT, exposure therapy, ACT (Acceptance & Commitment Therapy), mindfulness practices, and in some cases, anti-anxiety medications or SSRIs.
3. Bipolar Disorder
Bipolar disorder is marked by dramatic shifts in mood, energy, and activity levels. These shifts aren’t just emotional—they can affect sleep, decision-making, judgment, and even one’s sense of reality.
Types of Bipolar Disorder:
Bipolar I: At least one full manic episode (often followed by depression).
Bipolar II: Cycles between depressive episodes and hypomania (a less severe form of mania).
Cyclothymic Disorder: Frequent mood swings that don’t meet full criteria for mania or depression but still cause distress.
Mania may look like:
Feeling euphoric or invincible
Talking rapidly or jumping between ideas
Risk-taking (e.g., spending sprees, reckless driving, uncharacteristic behavior)
Reduced need for sleep
Depressive episodes may include:
Fatigue and hopelessness
Suicidal ideation
Withdrawal from loved ones or activities
Bipolar disorder is complex, and many people go years misdiagnosed as having depression alone. Proper diagnosis is critical because treatment typically requires mood stabilizers, not antidepressants alone.
Therapies that help: Mood-stabilizing medications, psychoeducation, routine regulation, DBT, and supportive psychotherapy.
4. PTSD (Post-Traumatic Stress Disorder)
PTSD occurs when a traumatic experience overwhelms the nervous system and leaves a lasting imprint. It’s the body’s way of trying to stay alert and protect you—even long after the danger has passed.
PTSD can develop after:
Physical or sexual assault
Combat or war exposure
Car accidents
Natural disasters
Childhood neglect or abuse
Medical trauma
Witnessing a traumatic event (even if it didn’t happen directly to you)
Common symptoms:
Intrusive memories, flashbacks, or nightmares
Emotional numbness or detachment
Avoidance of reminders of the trauma
Hypervigilance, exaggerated startle reflex
Negative beliefs about self or world (“I’m broken,” “Nowhere is safe”)
PTSD affects both the mind and body. Many people with PTSD also experience physical health issues, chronic pain, autoimmune symptoms, or digestive distress. Healing from PTSD often means retraining the nervous system and reprocessing the trauma safely.
Therapies that help: EMDR, trauma-focused CBT, somatic therapies, Brainspotting, and supportive group work.
5. OCD (Obsessive-Compulsive Disorder)
OCD is not about being “a neat freak.” It’s a serious condition involving intrusive, unwanted thoughts (obsessions) and repetitive behaviors or rituals (compulsions) that are done to relieve the anxiety those thoughts produce.
Obsessions might include:
Fear of contamination or germs
Violent or disturbing thoughts (e.g., hurting someone)
Doubts about having done something “right” (e.g., locking a door)
Religious or moral scrupulosity
Need for symmetry, order, or precision
Compulsions might include:
Repeated hand washing or cleaning
Checking locks or appliances over and over
Mentally repeating phrases or prayers
Avoiding certain numbers, people, or situations
Many people with OCD know their thoughts or actions don’t make sense, but the anxiety feels too intense to resist. OCD can be exhausting and interfere with daily life—but it’s also highly treatable.
Therapies that help: ERP (Exposure & Response Prevention), CBT, ACT, and medication (typically SSRIs).
6. Eating Disorders
Eating disorders aren’t just about food—they’re about control, self-worth, and coping with emotions in ways that may feel safer than expressing them outwardly. They often coexist with trauma, anxiety, perfectionism, or attachment wounds.
Types of Eating Disorders:
Anorexia Nervosa: Severe restriction of food intake, fear of gaining weight, and distorted body image.
Bulimia Nervosa: Binge eating followed by purging behaviors (vomiting, laxatives, excessive exercise).
Binge-Eating Disorder: Repeated episodes of eating large amounts of food in a short time, often with shame or guilt.
ARFID (Avoidant/Restrictive Food Intake Disorder): Highly selective eating or food avoidance not linked to body image.
Red flags may include:
Intense focus on calories, weight, or “clean eating”
Avoiding meals or eating in secret
Rigid rules around food, exercise, or body rituals
Physical changes like hair thinning, dental issues, digestive problems
Eating disorders can have serious medical consequences, including heart issues, infertility, and organ damage. But with compassionate, comprehensive treatment, recovery is possible.
Therapies that help: DBT, family-based therapy (especially for adolescents), nutrition counseling, trauma therapy, and medical monitoring.
What Affects Mental Health?
Mental health isn’t shaped by one factor—it’s influenced by a combination of biology, environment, and lifestyle. Here’s how they interact:
Biological Factors
Genetics: Some conditions run in families.
Brain chemistry: Neurotransmitter imbalances can affect mood and thinking.
Physical health: Hormonal changes, chronic illness, and even poor sleep can play a role.
FAQ: Can brain chemistry alone cause mental illness?
Not entirely—mental health is influenced by multiple factors. Medication may help, but therapy and lifestyle support are important too.
Environmental Factors
Exposure to trauma or abuse
Isolation or lack of social support
FAQ: Does childhood trauma always lead to mental illness?
Not always—but it does raise the risk. The right support can foster resilience and healing.
Lifestyle Factors
Diet and exercise: What you eat and how often you move can affect your mood.
Sleep: Poor sleep is a major contributor to anxiety, depression, and brain fog.
Substance use: Drugs and alcohol can worsen or mask mental health conditions.
FAQ: Can exercise really help?
Absolutely. Movement releases feel-good chemicals, improves focus, and boosts energy.
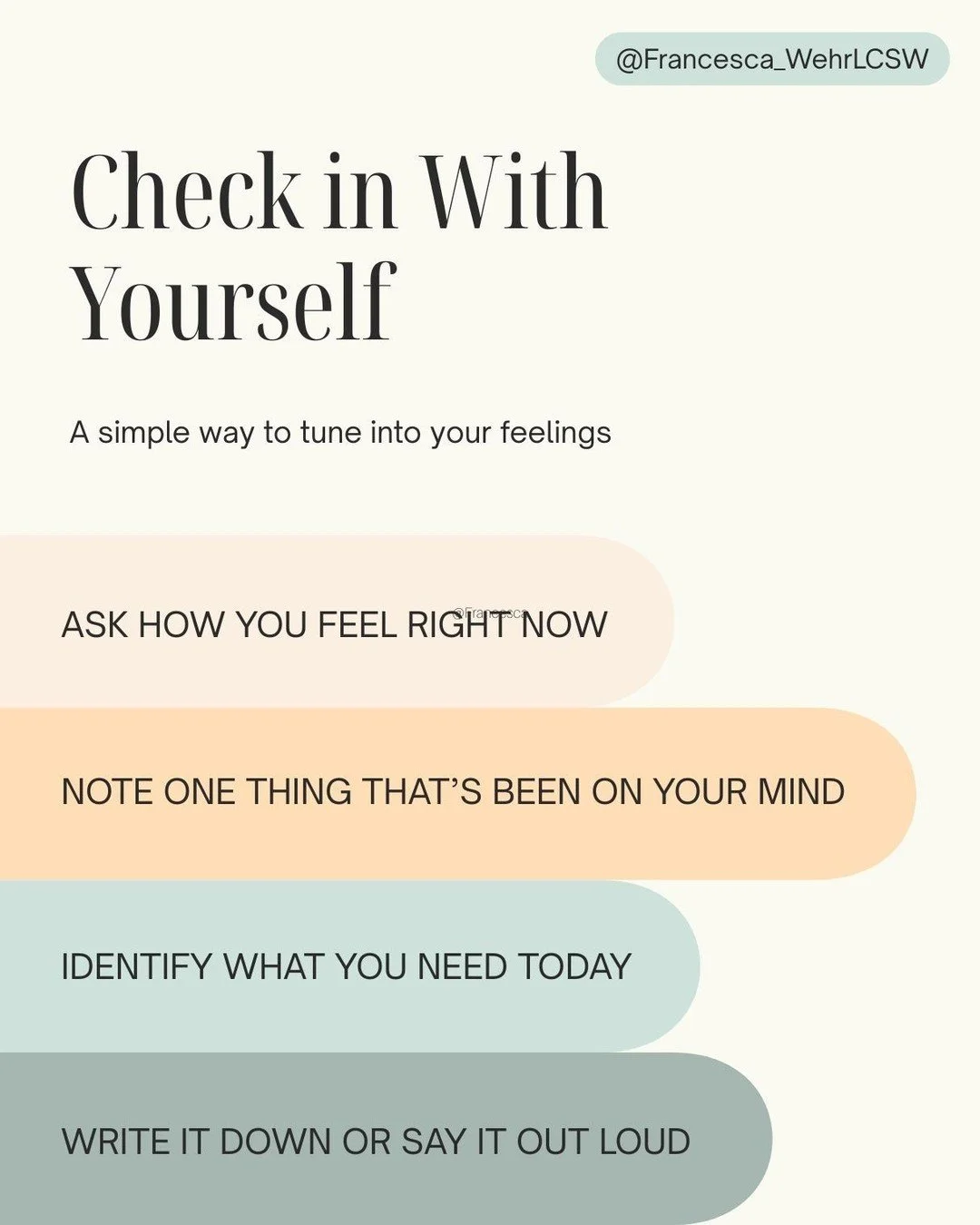
How to Take Care of Your Mental Health
Caring for your mental health doesn’t have to be complicated—but it does require intention. Here are three simple places to start:
1. Prioritize Self-Care
You don’t have to earn rest or joy. Self-care is how you maintain emotional fuel.
Try:
Setting boundaries
Taking screen breaks
Practicing mindfulness or yoga
2. Stay Connected
Human beings need connection. Reach out. Stay in touch. Ask for help. Join a support group or spend time with people who lift you up.
3. Seek Professional Help When You Need It
If your symptoms are affecting your daily life—or you just feel stuck—talk to a mental health professional. Therapy is not only for crises. It’s for growth, self-discovery, and healing too.
FAQ: When should I reach out?
If you’re wondering whether to get help, that’s usually a sign that you should.
Final Thoughts
Mental health isn’t a destination—it’s a process. It ebbs and flows, just like physical health. By learning the signs, knowing your resources, and taking care of your inner world, you’re already doing the work of wellness.
And if you're struggling, you’re not alone. Help is out there, and healing is possible.